Brain Injury Tests, Procedures, and Outlook for TBI Patients
Category: Personal Injury
Article by Aaron F. Tuley
Millions of accident victims suffer traumatic brain injuries (TBI) every year, and the effects can be as varied as the individuals themselves. Dealing with the possibility of a TBI can be overwhelming, but understanding the extent of your condition and your treatment options can provide clarity and comfort.
Immediate intervention and thorough testing are the most effective weapons to prevent long-term complications of TBI. Here, our experienced accident lawyers explore the most common testing methods to determine brain injury severity and the procedures that patients may need to overcome head trauma.
Diagnostic Tests for Traumatic Brain Injury
Whether a person has suffered a concussion or coma, the moments immediately following a head injury are crucial. Delaying or forgoing treatment can have drastic consequences on victims, so doctors and first responders need to assess a patient’s condition quickly.
Glasgow Coma Scale
Emergency medicine staff begin dealing with a possible brain injury by testing a patient’s responses using the Glasgow Coma Scale (GCS) as a guideline. The Glasgow Coma Scale grades a person’s abilities and responses after a head injury on a scale of three to 15. The lower the patient’s score, the more severe their injury.
First, the doctor will examine a patient’s eyes, studying the pupils, blinking, and eye response. The doctor sometimes can tell by the eyes alone if there is a brain injury. Next, they test the patient’s verbal and motor responses (if any). With each one of these tests, they give their patient a score that determines how severe their head trauma might be:
- Score of 8 or less – Severe Head Injury
- Score of 9-12 – Moderate Head Injury
- Score 13 to 15 – Mild Head Injury
After a doctor performs GCS testing, they move on to determine the severity of the injury using imaging tests.
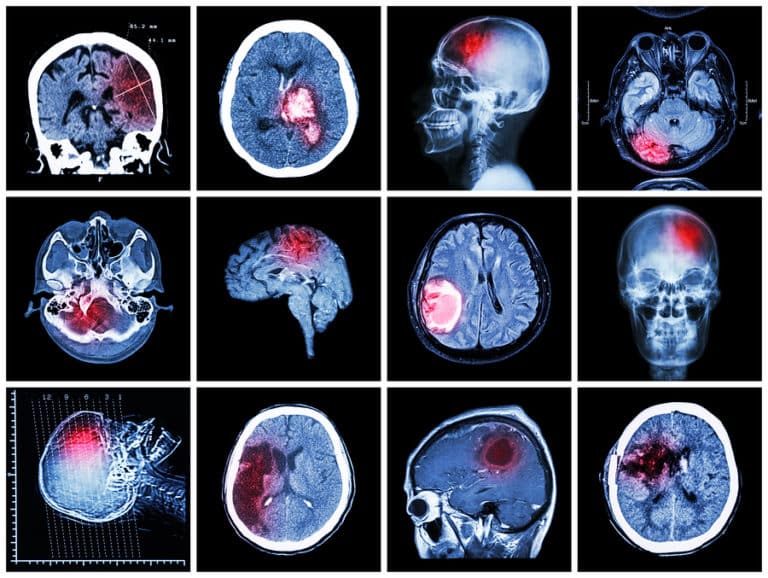
CT Scan
Computed tomography (CT) scans use X-rays to create detailed cross-sectional images of the brain, enabling doctors to see any abnormalities or damage. In cases of TBI, CT scans can reveal bleeding (hemorrhage), bruised brain tissue (contusions), blood clots (hematomas), swelling, fractures, or other structural changes within the brain. This information is vital for determining the severity of the injury and guiding appropriate treatment decisions.
MRI Scan
MRI (Magnetic Resonance Imaging) scans produce detailed images of the brain’s soft tissues using powerful radio waves and magnets. Unlike CT scans, MRI scans do not use ionizing radiation, making them safer for repeated use and ideal for detecting subtle changes in brain structure and function.
In cases of TBI, MRI scans can reveal more nuanced information, such as microscopic bleeding, diffuse axonal injury, inflammation, or damage to white matter tracts. This level of detail is crucial for understanding the extent of brain damage and predicting long-term outcomes. Additionally, MRI scans can help identify secondary complications, such as cerebral edema or herniation, which may require immediate intervention.
Intracranial Pressure Monitor
Swelling of the brain is a significant concern after head trauma because it can lead to secondary brain damage or even death. To guard against swelling, doctors may surgically insert an intracranial pressure (ICP) monitor to measure the pressure inside the skull. Elevated ICP warnings allow for early detection of bleeds, intracranial hypertension, or cerebral edema, enabling timely interventions.
Procedures for Patients With Traumatic Brain Injuries
A brain injury like a mild concussion may require no treatment other than rest, over-the-counter pain medicine, and monitoring for any change in condition. However, moderate or severe traumatic brain injuries might require hands-on hospital interventions, including:
Emergency Care
For moderate to severe traumatic brain injuries, doctors focus on stabilizing the patient’s condition and preventing further brain damage. Upon arrival at the emergency department, the medical staff constantly evaluates individuals’ neurological conditions and monitors their vital signs.
Immediate treatment centers on keeping the oxygen and the blood supply flowing, maintaining proper blood pressure, and preventing secondary brain injury. Doctors may implement measures to control seizures, manage pain, and prevent infections or blood clots.
Patients who have additional injuries, such as broken limbs or internal bleeding, need careful triage to determine which injury takes precedence. Transferring the patient to a specialized trauma center equipped with neurosurgical equipment may be necessary for further evaluation and definitive treatment.
Induced Coma
In some severe cases, doctors might decide to place a patient into a temporary deep sleep, known as an induced coma. Using less energy and oxygen helps the brain heal and protects brain cells from further damage. Doctors may induce comas using medication or by lowering the patient’s body temperature significantly (therapeutic hypothermia).
During the induced coma, medical staff closely monitor patients in intensive care units, with their body temperature meticulously regulated to prevent complications. While induced comas can benefit some severe TBI cases, healthcare professionals from various disciplines must carefully manage them due to the associated risks. The decision to initiate therapeutic hypothermia is based on the severity of the TBI, individual patient factors, and ongoing clinical assessments to minimize neurological complications.
Surgery
Sometimes, patients will need surgery to minimize brain damage or save the patient’s life.
Surgery carries complications, so it’s typically reserved for cases of severe trauma. Common types of surgery used to treat patients with TBI include:
- Craniotomy. A craniotomy involves surgically removing a portion of the skull to access the brain. This procedure is often performed to remove blood clots, relieve intracranial pressure, stop a bleed, or repair damaged brain tissue. During a craniotomy, neurosurgeons carefully remove the bone flap, perform the necessary interventions, and then replace the bone flap once the procedure is complete.
- Ventricular drainage. Patients suffering from cerebrospinal fluid (CSF) accumulation within the brain may need ventricular drainage procedures. This procedure involves inserting a catheter into the brain to drain excess CSF, lower intracranial pressure, and increase blood flow to the brain.
- Skull fracture repair. A break in the skull can cause bleeding, swelling, blood clots, or infection. Surgical repair of skull fractures may be necessary to stabilize the fracture, reduce the risk of complications, and promote healing. Depending on the extent and location of the fracture, patients may require cranioplasty (reconstruction of the skull) or fixation with plates and screws.
- Decompressive craniectomy. This surgery is usually reserved for patients with severe brain swelling where other measures to control pressure have failed. A surgeon removes a large portion of the skull to relieve intracranial pressure, allowing the brain to swell without restriction. While decompressive craniectomy can be life-saving, it may also be associated with complications such as infection, cerebral herniation, or long-term neurological deficits.
Traumatic Brain Injury Outcomes
Weeks After TBI
Once a patient is stable, doctors often prescribe medications to help them cope after leaving the hospital. The first is a diuretic to increase urine output, lessening the buildup of fluids in the body. The second is an anticonvulsant to prevent seizures.
TBIs can disrupt normal brain functions, leading to abnormal electrical activity and an increased susceptibility to seizures. Anti-seizure medications, also known as anticonvulsants or anti-epileptics, are prescribed to reduce the severity and frequency of seizures in TBI patients. These medications stabilize the electrical activity in the brain and prevent the spread of abnormal impulses that can trigger seizures.
Months After TBI
People who survive traumatic brain injuries will likely face ongoing follow-up exams, blood tests, and extensive rehabilitation. Depending on the severity and location of the trauma, a patient may need to relearn skills like talking, walking, dressing themselves, and performing everyday tasks. Speech therapy and physical rehabilitation are particularly frustrating for TBI patients.
The type and duration of rehabilitation varies but will generally continue until the patient can return to their daily routine or has reached a stage of maximum improvement. Some patients may experience seizures months or even years after the initial injury and need ongoing medication to keep these under control.
Years After TBI
Sometimes, severe brain injury can leave a patient in a coma for a prolonged period. Patients with widespread damage to the brain could be minimally conscious for years or left in a vegetative state.
Even after a successful recovery, patients may suffer long-term disabilities due to the following:
- Nerve damage
- Paralysis
- Memory lapses
- Cognitive problems
- Circulation problems
- Social problems
- Mood swings or behavioral changes
- Depression or mental health effects
- Sensory problems
We Can Help You Get the Treatment You Need
Our legal team recognizes the effects that a traumatic brain injury can have on you and your family. While you take the time to heal and rebuild your life, we take over the legal process, helping you get the compensation you deserve. Contact us today for a free evaluation of your case.
Have questions about your case?
Contact us
